Meaningful Use
The Medicare and Medicaid EHR Incentive Programs provide financial incentives for the “meaningful use” of certified EHR technology to improve patient care. To receive an EHR incentive payment, providers have to show that they are “meaningfully using” their EHRs by meeting thresholds for a number of objectives. CMS has established the objectives for “meaningful use” that eligible professionals must meet in order to receive an incentive payment.
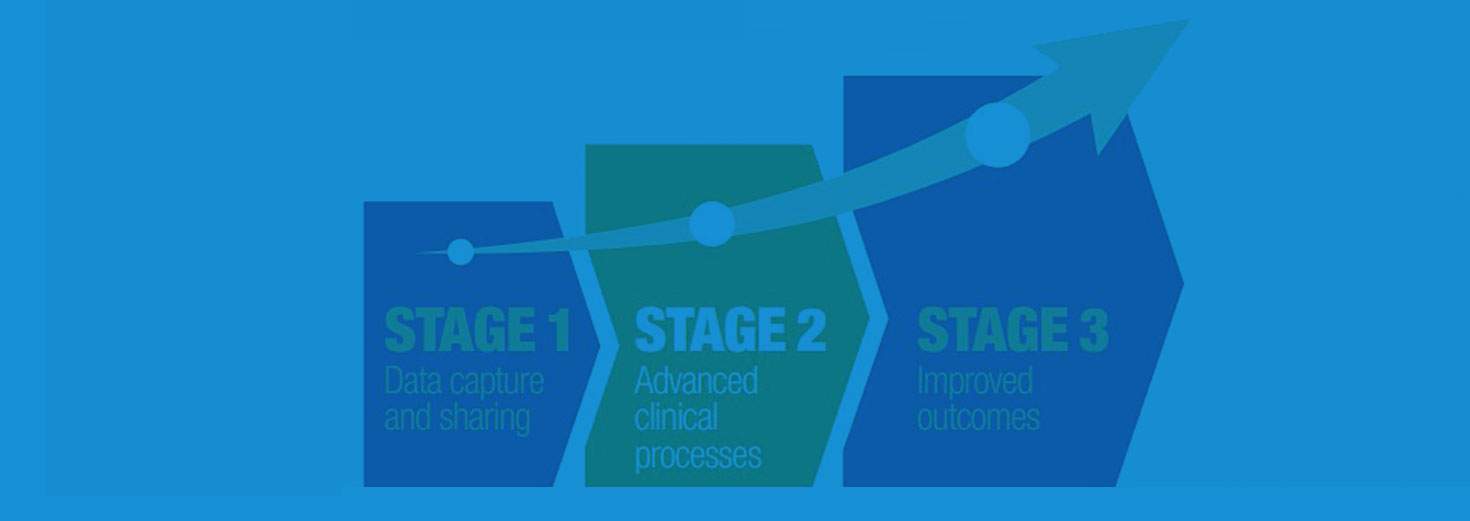
The Medicare and Medicaid EHR Incentive Programs are staged in three steps with increasing requirements for participation. All providers begin participating by meeting the Stage 1 requirements for a 90-day period in their first year of meaningful use and a full year in their second year of meaningful use. After meeting the Stage 1 requirements, providers will then have to meet Stage 2 requirements for two full years.
What is Meaningful Use?
Meaningful Use is using certified EHR technology to
- Improve quality, safety, efficiency, and reduce health disparities
- Engage patients and families in their health care
- Improve care coordination
- Improve population and public health
- All the while maintaining privacy and security
What are the Requirements of Stage 1 Meaningful Use?
Basic Overview of Stage 1 Meaningful Use:
- Reporting period is 90 days for first year and 1 year subsequently
- Reporting through attestation
- Objectives and Clinical Quality Measures
- Reporting may be yes/no or numerator/denominator attestation
- To meet certain objectives/measures, 80% of patients must have records in the certified EHR technology
Stage 1 Objectives and Measures Reporting
Eligible Professionals must complete:
- 15 core objectives
- 5 objectives out of 10 from menu set
- 6 total Clinical Quality Measures (3 core or alternate core, and 3 out of 38 from additional set)
- Applicability of Meaningful Use Measures and Objectives
Some MU objectives not applicable to every provider’s clinical practice, thus they would not have any eligible patients or actions for the measure denominator.
Exclusions do not count against the 5 deferred measures. In these cases, the eligible professional would be excluded from having to meet that measure.
Medicare and Medicaid Incentive Program basics
Medicare Eligible Professionals
The Medicare EHR Incentive Program for eligible professionals started in 2011, and EHR incentive payments under Medicare will continue through 2016. Depending on the first year they participate, eligible professionals can participate for up to 5 continuous years throughout the duration of the program. The last year to begin participation in the Medicare EHR Incentive Program is 2014. To receive the maximum EHR incentive payment, Medicare eligible professionals must begin participation by 2012.
Eligible professionals who demonstrate meaningful use of certified EHR technology can receive up to $44,000 over 5 continuous years under the Medicare EHR Incentive Program. See the payment table below for more information.
To qualify for Medicare EHR incentive payments, Medicare eligible professionals must successfully demonstrate meaningful use for each year of participation in the program.
Incentive payments for eligible professionals are made based on the calendar year. The reporting period for the first year is any 90 continuous days during the calendar year. The reporting period for all subsequent years is the entire calendar year.
Beginning in 2015, Medicare eligible professionals who do not successfully demonstrate meaningful use will be subject to a payment adjustment.
Medicaid Eligible Professionals
The Medicaid EHR Incentive Program is offered and administered voluntarily by states and territories. There are currently 45 states that offer the EHR Incentive Programs, and we expect the remainder to open their programs in 2012. (Check our Medicaid State Information page to learn which states are offering EHR incentives.)
The Medicaid EHR Incentive Program will continue to pay incentives through 2021. Eligible professionals can participate for 6 years, and participation years do not have to be consecutive.. The last year that an eligible professional can begin participation in the Medicaid EHR Incentive Program is 2016.
Incentive payments for eligible professionals are higher under the Medicaid EHR Incentive Payments— up to $63,750 over 6 years under the Medicaid EHR incentive program. See the payment table below for more information.
Medicaid eligible professionals can receive an incentive payment for adopting, implementing, or upgrading,certified EHR technology in their first year of participation. In subsequent participation years, Medicaid eligible professionals can receive incentive payments for successfully demonstrating meaningful use.
If you qualify for both the Medicare and Medicaid EHR Incentive Programs, you must choose which program you want to participate in. Find more information about the differences between the programs on our Getting Started page. Medicaid eligible professionals will not be subject to payment adjustments. However, Medicaid eligible professionals who also treat Medicare patients will have a payment adjustment to Medicare reimbursements starting in 2015 if they do not successfully demonstrate meaningful use.



